AcroTales
AcroTales
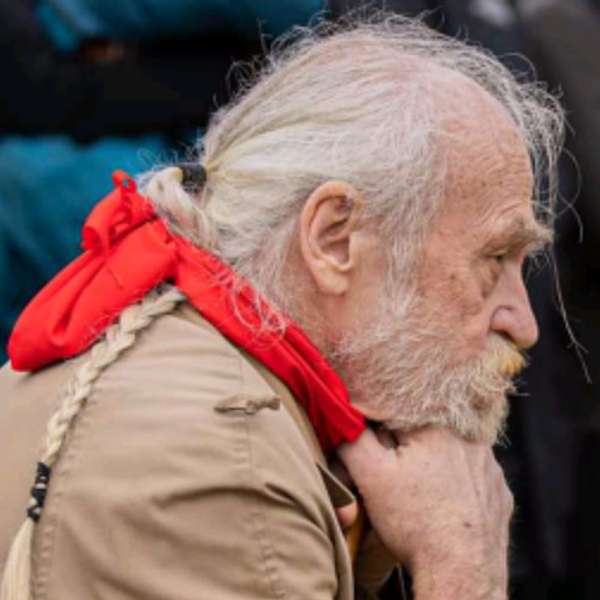
Episode 10 - Richard
Use Left/Right to seek, Home/End to jump to start or end. Hold shift to jump forward or backward.
In this episode of AcroTales, we hear from Richard in the UK. Richard was diagnosed in his mid-60s and talks about the diagnostic journey he underwent to reach his diagnosis and the impact it's had on his life, all told with great humour.
Hello and welcome to AcroTales, a podcast that explores the fascinating world of acromegaly. Acromegaly is a rare condition caused by a benign tumour in the pituitary gland causing an excessive release of growth hormones. My name's Dan Jeffries, and I was diagnosed with Acromegaly in 2007. And in each episode of AcroTales, I'll be talking to fellow acromegalics from around the world about their journey with this unique condition. It's episode 10, and I'm very pleased to welcome Richard from Exeter in the UK. Richard is 72 and was diagnosed with Acromegaly in 2011. Richard, welcome to AcroTales. Hello. So um we always start off this show talking about how you discovered that you had Acromegaly. That's normally the most interesting aspect of this. So um you would you you were obviously diagnosed in uh when you were about 61, which is quite late, I think, for people with Acromegaly. So maybe you could just tell us your journey about how you got to that point.
SPEAKER_02:Um it started in December 2010 with on a different condition. I had um what's the word? Uh neuralgia. I had a pain in my leg, which you know, a trapped nerve which crippled me for best about six weeks.
SPEAKER_01:Right.
SPEAKER_02:And um I'll make a comment about the medication later on on that one. I got off that, I got over that and went back to work. And um almost the first day back, oh uh that time I was working in an office for local authority, sitting down most of the time with a computer. And halfway through the first day, by lunchtime, I realized I just couldn't go through the day. It came out, you know. Uh this is the strangest thing about my condition, it just seemed to hit me out of the blue.
SPEAKER_00:Right.
SPEAKER_02:Took the rest of the day off, and then it didn't seem to get any better. Fortunately, because of my employer, I was able to work half time. I negotiated that, they had a welfare department, health and welfare department that helped me out, and I tried to find what was going on. Um the first thing that came to mind was that you know this lack of energy. I'd experienced was before when I'd had had hepatitis and getting over that. And um I f had you know witnessing my GP had my liver checked, and nothing wrong with it. So I had other checks and nothing couldn't cut him up. And at one point I was saying that fit, I should be up for the Olympics. Um and this went on and on and on and took various tests. Um going alongside of this, I'd actually managed part to collect um uh what do you call it? A hernia. Which took some time to diagnose because my my doc my GPs couldn't find it until it was a scan, and then that was but on hold. That's a whole side story, but it just goes along in parallel.
SPEAKER_01:Yeah, they're kind of connected, I would imagine. Yeah.
SPEAKER_02:Could well it had more to do with the fact that I've been on coding phosphate for for six weeks, and I'd recommend if you do that and take an um that uh what do you call it? Um loosener, bower loosener.
SPEAKER_01:Uh suppository, yeah.
SPEAKER_02:Well, and then any kind of thing to to loosen things up. Um anyway, this went on the the actual to tr getting a diagnosis took nine months. Right.
SPEAKER_01:Okay.
SPEAKER_02:Which from what I gather is not too bad. No. But uh during that time, um my energy levels were going down and down and down. And one of the first things I realized was, and I don't know how to describe it new, but it's to tie in with the thing about hepatitis. I knew I couldn't process protein.
SPEAKER_01:Right.
SPEAKER_02:Um, I don't remember any incidences of you know bowel disturbance or throwing up, whatever. I just knew my body couldn't handle it. My diet got more and more restricted. Um at one stage I was assessed for ME, which was just an interview with a trainee psychologist, which I realized, you know, in the end I gave up on that. I said, no. This I know this is physiological, physiological, this is my body, uh, this is not a psychical problem. I've I lived with someone who had ME, I have no uh previous um infection, it's nothing like ME, it's something completely different. And this went on and on and on right through the summer. By the middle of the summer, I was struggling to get by. Um I said in my memoir, my at the end, I was virtually living on Complan, which is a dietary substitute, yeah, porridge and multivitamins and nothing else.
SPEAKER_01:Right.
SPEAKER_02:Um getting around was really hard work. I mean I live fairly close to the central town, but the bottom of Deep Valley, which used to be part of the city's northern defenses. So every day I go into town, I attack the city. Um getting I was even coming back from the shops, I was had to work this out in number of steps, splitting up the distances into fractions is how far have I got? Can I make it? And really feeling in pain at times, you know, like more than 200 meters was very, very hard work. So this went on. But I was still at work and still working half time, just about managing that. And then one day in August, um working with a computer screen, and I kept on thinking my glasses, because I now wear clot glasses, were mistered up, great gr grimy. So I'm polishing the gro my glasses for the length of time and close my left eye and look to the right eye to see if we look clear. And I realized the sense of my vision was grayed out. And I thought that's age that's not right. That's age-related macular degeneration. Right. And this was literally just before the August Bank holiday.
SPEAKER_00:Right.
SPEAKER_02:So I go to the the uh my local chemist for they have an optician optical optician service. The guy looks at the woman looks at my eye and says, You've got an inflamed nocturne nerve, you better go to A. I thought, August Bank holiday, no, thank you very much. Backed out. And then I found out that that we had an eye hospital, part of our hospital, and they had their own AE, and I went in on the Monday, and this young intern looked in my eye and said, No, you've always had that since you were born. The problem's the problem's further in. But that's my brain. Oh shit. Um so he then put me for a I think the first thing was an MRI scan. And um this was probably beginning into September by now. And um that was inconclusive. Well, not conclusive enough. They called me for a CT scan and told me it was from a purity gland. I went to school at a grammar school many, many decades ago, and one of the f one of the things we did if we did we but we did biology for one year, and one of the things we did was endocrine glands, so I knew about what they were and where my. Oh. Oh yeah. For acromegally? No, for a paturity tumor.
SPEAKER_01:Oh, for right, okay.
SPEAKER_02:So it's not just acromegaly that is, as you know. And there are other glands, uh, the the thyroid, uh, the adrenal glands, many others can be affected by this condition.
SPEAKER_01:Yes, no, of course, yeah.
SPEAKER_02:And they you know go different ways, you know, too much or too little or whatever. And we're all paturity people in a suffer is a whole range of different conditions. Um, so okay, fine. Now we have a diagnosis. Um the next thing I'm called in, this is probably mid-September to meet the team. Now, the Royal Devon X and Hospital, which is not far from me, it's a bus ride and a walk away from here. Had a joint team with a big no big clinical hospital in Plymouth, where they had a neurological team that specialized in this. And I met the team and I talked to them and I said, Well, you know, um, what are you gonna do? So I'm gonna go in and cop operate on it. I said, I said at the bottom of my brain, I'm gonna do it, you gonna take my brain out? He said, No, I'd work through your nose. Oh, lovely. I've had operations in my nose before, and I did not want another one. And I said, Well what happens if I don't have it, and he said, Well, you'll probably go you'll blow you'll go blind and probably die. I thought, okay. I'll have the operation in that case. Yeah, I'd better have it then. Um I was in hospital in ten days later.
SPEAKER_01:Wow, that's pretty quick. It was. Um Did they tell you how big it was? No, but I found out afterwards. Right, okay.
SPEAKER_02:And um this um neurosurgeon, well name his name was Louis Lou or Louis Popareskin, he was an American. Right originally. And the morning after the operation he came around to see me to see how I was, and I was astonished. I'd never ever seen a a consultant come to see a patient after the operation. Right. He became a hero there in Ben.
SPEAKER_01:Yeah, yeah.
SPEAKER_02:Um I was in the hospital three three days after the op. I got was taken ambulance back home. Um still feeling pretty weak. My brother, who lives in the next county, picked me up and I stayed with him about six, seven weeks to recuperate. Um what happened after that is that well, the one of the first things that happened after that was I was put on hydrocortisone. Uh I think it was the only thing at first which brought my appetite back instantly so I could eat.
SPEAKER_01:Yes.
SPEAKER_02:Um and I met my um special specialist at the centre. Um she was a star as well.
SPEAKER_00:Okay.
SPEAKER_02:Um then came then kicked in the whole business of d dealing with the hernia and um which hadn't been dealt with for reasons I won't go into. And I was told I couldn't have I was operation booked for the following spring, which I couldn't have because I my heart my thyroid levels are too high. Uh I was given when that came down, I was prescribed pyrthyroxine to stabilize it. Had that operation. And then I think April I started um radiotherapy. I had five weeks of that, five days a week for five weeks. Right. Which is very weird. Radiotherapy for the tumor. Is that what was left? I asked I asked his consultant if they'd cut it all out. He said no, because too much it you know, it was a stage where it was too I d I thought they had cameras with them. I don't know if they do have an endoscopic candle with a camera when they're doing this, but he said it was too close to an artery. So he took out what he could and then and pulled out. Uh the radiotherapy. Um I've had I've I've actually got uh pictures of I think it's the first MRI scan, or maybe the first CT scan. And uh before they operated it was about the size of a like an old marshmallow, about two centimeters cube, it looks like they look much the same thing. Um I haven't seen pictures since because they want me to pay for them and I'm I'm too tight-fisted.
SPEAKER_01:So you're kind of like borderline macro, I don't know.
SPEAKER_02:I would say I would say it was a macro, but I don't know, it was at least two centimetres, two and a half centimetres cube.
SPEAKER_01:And do you do you have any I mean you had no idea this was growing? You had no inclination during your 40s, 50s, 60s that really that's I said as I wrote to you, um in retrospect, my knuckles might have got thicker.
SPEAKER_02:Right. Um, but I thought I was just down to you know my work, my feet might have got larger. Again, I thought uh when I got measured to realize I was a size I was wearing shoes a size too small. I thought maybe I just got it wrong in the first place. I was being optimistic.
SPEAKER_01:Um facial changes? Did you had to do it?
SPEAKER_02:My my endocrinologist says yes. I couldn't. I can feel what I feel it almost feel like I don't know if I keep meaning to check my brothers, if they got them because we're very similar. I've got two brothers. Well it feels almost like I got horns budding at the edges of my eyebrows.
SPEAKER_01:Okay.
SPEAKER_02:Um I've I've seen pictures of other acromagellics, as you call them, you know, in movies, the famous ones like Jaws and the others. Um what's his name? The guy from the mu uh monsters, yeah. Um you mean. So I I couldn't see it, but it might consult them good.
SPEAKER_01:That's really interesting then, because you know, we've uh often with the tales, people generally feel like a sort of steady decline in their well-being and uh and it can get picked up for other reasons, and that is kind of what happened to you, but maybe not quite as extreme. And um, you know, who's to say it could have been growing? It's hard to know. I think if it's two centimetres, you've got to assume it's probably only growing for maybe six, seven years.
SPEAKER_02:I asked people that say it said maybe four or five, so right. Okay. What triggered it? They don't seem to have any ideas at all.
SPEAKER_01:No. And so after the surgery and the treatment, how did you feel? Did you did you feel a lot better? Did you had it like like your life turned around? What was the outcome of that?
SPEAKER_02:Well, I've had a few things happen to me which have turned my life around, so that was uh it wasn't a new experience. Um this was it was scary. I mean, one of the first the thought of someone operating my brain my brain scared me, and I actually sat down and wrote my will.
SPEAKER_00:Right.
SPEAKER_02:First thing, which I had put off. Um coming out of it I felt a whole lot better. First, getting my appetite back, building my strength back up, and my muscular strength. That was better. I mean I've been I've had a very varied life, mostly I'm not an athlete but sort of fairly active. Okay. And um one of the things which messed me up more and they may have disguised it was about uh back in uh twenty odd years ago, I had a fight with a bicycle thief, idiot, and um ended up having the head of my fever cracked. Right. Um, which didn't heal, and I've now got a half-bit replacement. So that slowed me down an awful lot. I mean, I'd say in my early 50s I was fit in a lot of people in their 30s. Right with a cash potato variety. After that, I was a lot slower.
SPEAKER_01:Right.
SPEAKER_02:Um so I may not have noticed any in a other changes.
SPEAKER_01:I see what you mean. Okay, I I I understand that. Um okay, well that's that's really interesting. And then uh so I know that we've you mentioned that you kind of got involved with working with paturity support on s on some levels. How did that come about?
SPEAKER_02:Well, there is in the UK the Purity Foundation. Um I was told about that and got in touch. I mean, early on when I was trying to work out, you know, is at the beginning you you're very conf confused, I don't know. I mean you have lots of questions, but it's not a good idea.
SPEAKER_01:Yes, yes, of course.
SPEAKER_02:And they have a telephone body service, and I got in touch with a couple of guys who had not the same conditions but had been through that some of that experience, and that was a bit reassuring, so I thought that's cool. So I I'm actually a member, you know, it's there. Uh some people I know this. Some people need it more than others. And they told me there there was a support group based in the southwest. And um I'm I'm sure there's others around the country. This guy based in he lives in Plymouth, who's organized them in around hospitals in Plymouth. Um he's not in Plymouth, in Cornwall. So he's in Truro, Plymouth, Torquay, Exeter, Cornwall and Devon, and Taunton in Somerset. So we meet twice a year, all kinds of people with different different maturity conditions, and we chat.
SPEAKER_01:Excellent.
SPEAKER_02:And mine is at the local Exeter hospital. The person who's nearly practically every time I've been there is the head of the endocrinology, a woman doctor, who answers all our technical questions and is usually a Well that's just invaluable, isn't it? It is. I I mean, I don't say it's helped me a lot, but you know, just it's good to have that feeling that there's other people around who can understand what you're going on, that you're going through, and to help them as well, to give them the support.
SPEAKER_01:Because I think also you may not see your endocrinologist for a year, maybe two years, and then when you are seeing your endocrinologist, you forget the questions to ask, and then and then this kind of gives that opportunity that if something has happened in the interim uh between your your session, you know, your your traditional appointment as such, then you know you can discuss stuff and discuss it with other people.
SPEAKER_02:I I meet my endocrine my my particular endocrinologist who's um a professor and he's Nepalese, lovely blow. Okay. Um we generally meet twice a year. The last time we did it on on we did a screen talk.
SPEAKER_01:Uh screen sharing, right? Okay.
SPEAKER_02:Um that's in the go okay. Um I you know, if I have questions, I generally make a note of them and and he's you know he answers them if he can. It's good.
SPEAKER_01:Okay, so Richard, if you uh had met somebody that just been diagnosed with acromegaly, what would you what would you say to them? What would be your advice for them? Oh um well it depends what stage they're at.
SPEAKER_02:Presuming they've been diagnosed, they've got medical support. And hopefully it's medical support they can afford. Yes. Um we have an NS in this country for the moment. If we can stop these uh gangsters and governments from selling it off to the Americans. Um no offense to Americans, but your corporations are evil.
SPEAKER_01:Yes, it's slightly more.
SPEAKER_02:Silver hours for that matter, but there you go. But you know.
SPEAKER_01:Yeah, but nobody wants the NHS sold off, especially when you know how much amazing work it's done for you, you know, saved our lives, people with acromagolite to an extent. And you think of how complex that treatment is and that surgery is and the aftercare that goes with it. And it's you know, I think we're forever indebted for the service that we get. I'd be I'd be dead. Simple as that. You know, this is what you you were in you were admitted ten days after they discovered it, you know. That's it's incredible.
SPEAKER_02:Well no, ten days after the consultation. I mean, they discovered maybe a few weeks, but ten days after that consultation with the team, I was in surgery. Yeah. Um one thing I remember my the the um support nurse I I first had, she's moved on, said you know, when I came in, she said, I'm surprised you didn't come in as an emergency payment patient. You look so bad, you know.
SPEAKER_01:Thanks so much.
SPEAKER_02:But that's what I felt like.
SPEAKER_01:But this is what's so amazing about this condition is it can just sit there dormant, and if and potentially if you weren't experiencing other issues, you may have not gone in for to get those checked, and you may have not had the acromegaly discovered for 10, 15, 20 years, and by that time it can play massive havoc on your life. So uh it's you know, these things happen, I guess, for a reason, but it's uh it's just amazing. Every story is completely unique in terms of the discovery and the uh and and the eventual diagnosis of it.
SPEAKER_02:So that is the hard part because it's so rare. I mean, you know, no no one in in my GP surgery, and it's quite a large one, had ever come across anything like it. They were completely clueless. And uh, I mean, I've become an expert at managing my condition because I you know I know more about it than they do, and I'm negotiating between them and the and the hospital.
SPEAKER_01:Yeah, well, we we become our own pa we become patient experts and we and we we have to manage our own pathway because if we sometimes left it in the hands of those that don't quite know what we're going through, we wouldn't get the results that we wanted.
SPEAKER_02:If you say, you know, but I would say that someone's been diagnosed, well done, because I know you've had a hard job so far, you know. So carry on from there, you know. Yeah, take control, you know, it's your health. Um you tell them what you need.
unknown:Yeah.
SPEAKER_02:Um my my I'm on it. I said I cheer my whip my women friends up by saying I've got constant PMT. That's what it's like living with because you know the the I'm and I take you know uh hydrocortisone, levi thyroxine. I have 12 weekly injections of um testosterone. Test the NMBT. Um I've got another one doing coming at the end of this month. Um do you find it helps? I'd be pretty messed up without it, I suppose. Um it's testosterone. I could talk about testosterone until the towers come home. It's not what everyone assumes it's like. It's it feels like almost the opposite. We've been passing that within them in other time, but um, you know No, I no, I think you're right.
SPEAKER_01:I think everyone thinks you imagine you turn into this ogre with like big hairy hands, and you know, you become this raging stallion. It's not, it's kind of it's it's it's almost leveling, and it's more about confidence and the ability to function.
SPEAKER_02:I can't t I can't really tell. I mean, um, you know, the first time I got it, I thought it might give my biggest problem that always has been is motivation. I mean, my I do suffer a lot from fatigue. Getting motivated to do something is look around my little flat here, and there's so many things I should be doing. I just and then if I start, I'll just give up at some stage. It just wouldn't have the energy to go through it, or if it will it'll knacker me. Um first time I got the testosterone, I thought I might cure that, but it didn't. And the cu most curious thing about it, you know, people to testosterone driven. I'm actually horny about the end of the the 12 weeks in the beginning. Go figure. Um but it is you know, because you got this injection that is slow absorption. It is slow releasing, it is uh it's very strange, it's not at all what people assume it is. Um but for the acry for the acromegli, what I take is cabergolin.
SPEAKER_01:Okay.
SPEAKER_02:Uh I was originally on Smashulin or Namio Tard, whatever you call it, injections, monthly injections. And that was such a ride. Um I describe it as like being on an emotional um switchback for the Americans or roller coaster for the Brits.
SPEAKER_01:Yeah, yeah.
SPEAKER_02:Up and down, up and down. Um, I mean I'd I I'd say that I'm not a man who's so severely screwed down. You know, I could get emotional, I could weep out time. These days, anything can get me teared up. You know, I can get filled, you know, in grief just looking down in my fridge. I'm thinking, what the I'm only looking down for some what's in the fridge. What's going on? Um it is very strange. You know, hormones. I I've looked I've looked online at hormones and what they do, and you know, the system is so complicated.
SPEAKER_01:It's crazy.
SPEAKER_02:I you know get a brain ache just trying to read it. And um so the the medication replaces it, but it's a very rough and ready, you know. But yes, they take the measurements and they try and tailor them from within their what they think are the safe limits, but it's not what you began with. In some ways it might be better if we all had a good idea what our hormone levels were before we got ill. Yeah. Of course. You know, then they could tailor them more precisely, but that's not possible.
SPEAKER_01:And I also think sometimes I I always wonder how much of it is hormone and how much of it is it just our natural personality? It's it's how do you tell the difference? Well, sometimes you can, but I think you know, uh if you're having a bad day and you're just feeling low, or if you're feeling incredibly excited, or whatever, is that necessarily a production of your hormones, or can that just be just who you are and how your personality traits come out in different ways? You know, I I I appreciate their links, yeah. There's no kind of question about that, but it's very hard to know.
SPEAKER_02:Um it is a balance between the two. I mean, y yes, it's about like genetics, you are not your genes, but they influence what happens. I mean, I put it at one stage I theorized what would happen. I asked my consultant the possibility of a transplant of of my of my pituitary gland. And I thought, well, if I did, would I become that other person?
SPEAKER_01:Yeah.
SPEAKER_02:Um, or would my history balance that out? And it it's a mixture of both, it's a mixture of history and your hormones and your emotions. You can it's very difficult to override your emotions because they are when in you know you're taking these kind of levels of medication, they are so strong, they really hit you. So for new people get used to it, you know, be prepared. Uh my one of our last meetings, I met a guy who was you know I can't remember what he was diagnosed with, but he had a recent diagnosis and he said he'd he'd obviously been a very active guy, physical well, where he said he was almost suicidal. You know, okay, it's tough, but you can get it through it, you can live with it. Yeah. You know, it does change your life, but it's culpable.
SPEAKER_01:I think on that positive note, you can get through it. I'm gonna call this uh conversation to an end. Okay. Richard's been absolutely fantastic chatting with you, and I think you've offered some really interesting insights and you know, pearls of wisdom for those who are diagnosed with this condition. So um I'm very grateful for you taking the time to talk to me today.
SPEAKER_02:Thank you, and you're doing a good job yourself. Thank you.
SPEAKER_01:Uh thank you very much. Well, if you found Richard's story interesting and you want to hear other Acrotales, head over to Acrotales.com or just search for it in your favourite browser uh and you'll find the ever-expanding library of interviews. And of course, you can also subscribe to the podcast to receive the latest updates. And that you can do that via iTunes and Spotify or your favourite RSS feed, whatever you want to use. So, once again, big thank you to Richard, and we'll see you next time for another acrylic show.